
As the opioid epidemic was worsened over the years, the need for opioid addiction recovery methods has also increased. According to the 2018 NSDUH Annual National Report, a whopping two million Americans (over the age of 12) suffer from an opioid addiction in some form. This is a concerning number, and it’s important that the healthcare industry sufficiently accommodate those in need of recovery from opioid addiction.
The Truth About Opiate Addictions and Opioid Addiction Recovery
Opioid addictions don’t come in just one shape or size. A variety of drugs fall under the opioid class, but what do all of these drugs have in common? They are all highly addictive, leading users to quickly develop physical and psychological dependence. If this dependence is not satisfied, then severe withdrawal symptoms can be the result. Due to these withdrawals, it can be especially difficult to pull oneself out of an opioid addiction, especially an addiction that has developed over a substantial amount of time.
Effectively treating opioid addiction isn’t an easy task. Whether the individual has developed a dependence upon heroin or a prescription painkiller (such as OxyContin), recovery is rarely quick and simple. Rather, recovery is a gradual process, which involves several important steps. The earliest stage of this process is known as the detox phase, and this is often the period in which an individual may utilize a medication such as Suboxone or methadone.
Although these drugs can be useful to dampen opioid withdrawals and curb cravings for a short period of time, they should never be used as long-term solutions. In reality, the goal of recovery isn’t to replace one drug addiction with a new one. Medications such as Suboxone are highly addictive, and over time, can lead someone to develop an entirely new drug dependence. This is highly counterintuitive to the goals of substance dependency recovery.
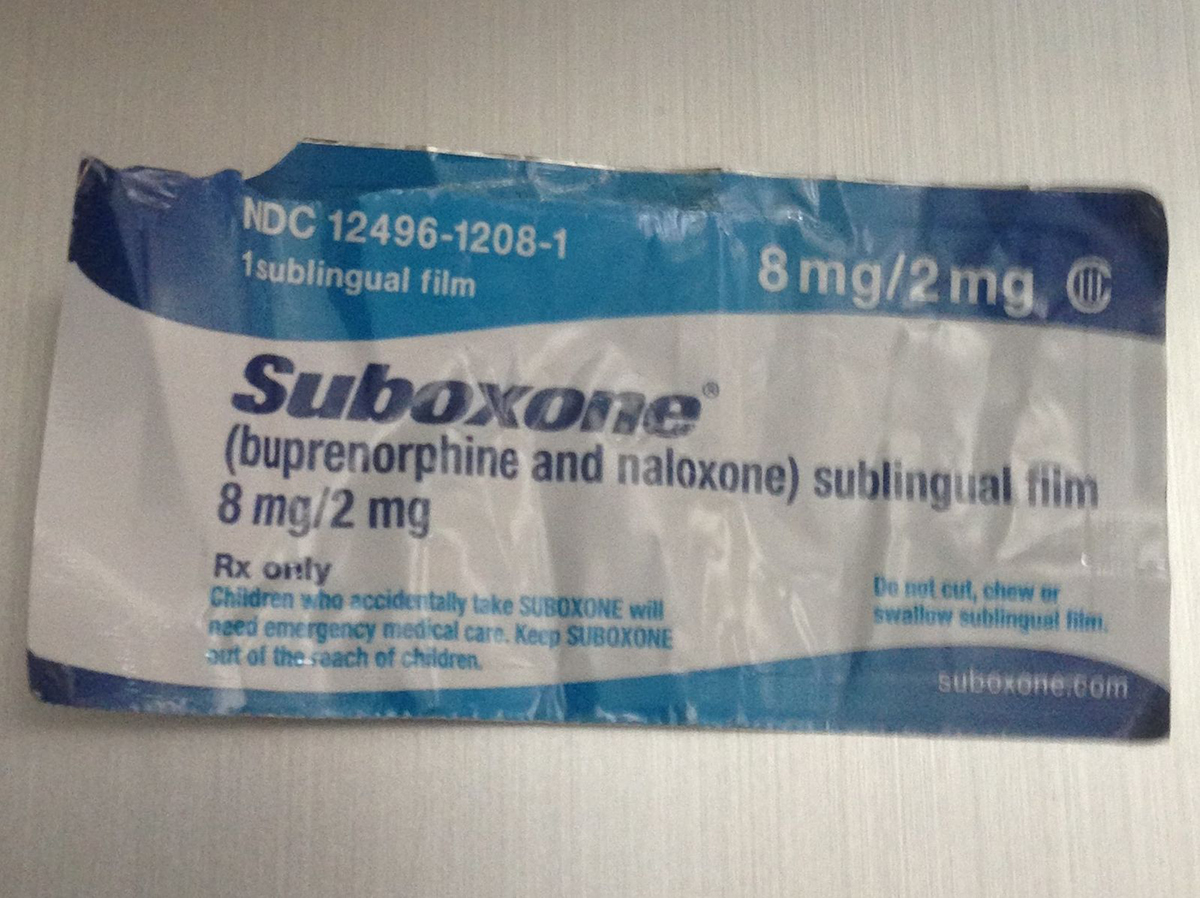
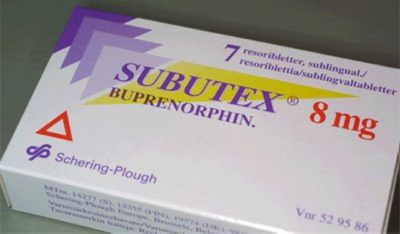
What Is Suboxone?

Supertheman, CC BY-SA 3.0, via Wikimedia Commons
At this point in time, three medications have been approved by the FDA to sufficiently treat opioid withdrawal symptoms. These medications are buprenorphine, methadone, and naltrexone. Each of these drugs has proven effective at reducing or de-intensifying withdrawal symptoms, as well as providing users with milder and more manageable cravings.
Keep in mind that of these three medications, two are actually opioids, in their own right — buprenorphine and methadone, specifically. For this reason, the administration of these medications is not taken lightly. If someone is put on a regime of either buprenorphine or methadone, they can expect heavy monitoring from their doctor. Additionally, due to the physically and psychologically addictive qualities of these medications, they are rarely used for long stretches of time, as this can only lead to new problems. Overdose and addiction are a risk in either case.
Well, then, what even is Suboxone? How does this medication fit into the realm of opioid recovery?
In truth, Suboxone is a combination of two separate medications, being buprenorphine and naloxone. Buprenorphine, specifically, is known as an opioid partial agonist. Essentially, this means that it will only partially block access to the body’s opioid receptors, should the individual consume another kind of opioid drug. Once it successfully binds to the opioid receptors, buprenorphine will lead the user to experience a mild high. This is a long-lasting and strong effect, leaving the individual unable to experience the euphoric effects of full opioids, should they consume them. This is often an effective way to curb cravings and potential relapses.
Naloxone is a bit different. This drug is an opioid antagonist, which means that it is able to fully block the brain’s opioid receptors. In addition, naloxone is able to work in opposition to the effect of opioids within the brain. This basically means that the user’s high will be prevented altogether. Once this occurs, however, the individual can expect to experience immediate withdrawal symptoms. This isn’t a pleasant experience and serves to discourage naloxone and Suboxone users from misusing the medication.
Compared to methadone, Suboxone is just about as effective in suppressing opioid cravings and subsequent abuse. However, Suboxone is typically considered to be a safer option, leading it to be desirable as far as medication-assisted treatment goes.
Still, like all medications used to treat opioid addiction, Suboxone is far from being without its flaws.
Suboxone Side Effects
GamblinMan22, CC BY-SA 3.0, via Wikimedia Commons
The side effects of Suboxone can vary quite a bit in their severity. Some individuals may experience mild symptoms only, while others can be hit with some of the more severe, disabling side effects. When Suboxone is used for extended periods of time especially, users will often experience significant side effects.
In terms of Suboxone’s milder, more common side effects, users of the medication might experience:
- Symptoms of opioid withdrawal, including abdominal cramps, body aches, and increased heart rate
- Headaches
- Depression and/or anxiety
- Insomnia
- Increased sweating
- Nausea
- Constipation
- Redness within the mouth
- Weakness and fatigue
- A burning sensation on the tongue
- Back pain
This is not a complete list of potential side effects of Suboxone, although these are some of the most typical. They can also occur with different levels of severity; while one user may experience mild headaches, for instance, another Suboxone user could end up suffering severe migraines. If any of these side effects become severe, it is important to bring this up to your doctor as soon as possible.
While severe side effects of Suboxone aren’t especially common, it is still possible for them to occur.
Some of these less common (and typically more severe) side effects include:
- Dependence and abuse.
- Hormonal problems
- Severe allergic reactions
- Breathing difficulties
- Coma
- Severe withdrawals
- Liver damage
Again, if you ever begin to experience severe or even debilitating side effects when taking Suboxone, consult with your doctor immediately.
Common Issues of Getting Off Suboxone
When patients adhere to a careful Suboxone maintenance model, it is less likely that they will struggle to come off the medication. If Suboxone is only taken for short durations at a time, it is far easier to avoid the development of a new dependency or addiction. Additionally, as with most medications, those coming off Suboxone should taper their dose down over the course of several weeks. It is not typically a good idea to stop the medication abruptly, as this can lead to more issues coming off.
If the individual has developed a dependence on Suboxone, then they are likely to experience withdrawals coming off the medication.
Potential Suboxone withdrawal symptoms include:
- Headaches
- Nausea
- Insomnia
- Muscle aches
- Diarrhea
- Irritability
- Anxiety
- Excessive sweating
- Drug cravings
As you might have noticed, the withdrawal symptoms of Suboxone are remarkably similar to those you’d expect to see from other opioid withdrawals.
Suboxone Abuse and Addiction
ZngZng, CC BY-SA 3.0, via Wikimedia Commons
Interestingly enough, Suboxone has been deemed the least abused opioid in the United States, compared to all others that were tracked. Although this is certainly a positive characteristic of the drug, it is vital that users don’t let this cloud their judgment. Just because Suboxone features a lower risk of addiction and abuse in users does not mean that it’s a wise idea to take the medication for long stretches of time. The longer you take Suboxone, the more likely it is that you’ll develop a physical and psychological dependence on this medication.
Sometimes, individuals may even use Suboxone illicitly. If you are taking this medication, it’s crucial that you do so under the watchful eye of a doctor — this is the case for any drug used to treat or manage opioid addiction. However, when a person chooses to self-medicate with Suboxone, they no longer have this buffer, guiding their Suboxone usage. Without these limits in place, not only is disaster more likely to occur but there will be no one to intervene and stop the user from traveling down this dangerous path.
Illicit Suboxone use typically begins as a means to self-treat the difficult symptoms of opioid withdrawal. Still, without the proper medical supervision, this situation can quickly spiral into an entirely new addiction. In that sense, the user is essentially replacing one dependency with another. This is not a solution to the problem — it is an entirely new problem, instead.
Further, if illicit Suboxone is taken via injection, this puts the user at even more severe risk. Whenever someone opts to inject themselves with Suboxone, they are at risk of developing infections and abscesses. Additionally, there is even a chance that they could develop a blood-borne infection, including hepatitis and HIV.
Signs of Suboxone Abuse
While Suboxone addiction is sometimes the result of illicit administration, this often isn’t the case. Much of the time, instances of Suboxone abuse occur after the patient is prescribed the medication by their doctor to treat opioid withdrawal symptoms.
It’s vital that any doctor prescribing Suboxone (or similar drugs, such as methadone) be highly trained in the treatment of substance abuse. Whenever the healthcare professional isn’t fully trained, it’s far more likely that mishaps will occur due to the doctor’s insufficient understanding of Suboxone’s properties and risks. For instance, a doctor could prescribe Suboxone to patients as a long-term treatment, not understanding just how risky this truly is. They might also not have the resources or experience needed to monitor the patient’s progress.
So, how can you tell if a legitimate Suboxone prescription has developed into a dangerous dependence? As with other addictive prescription medications, it’s important to look at the user’s behaviors. For example, is the patient going through their supply of medication faster than they should be, based on the prescribed dosage? Are they acting secretive, or even outright lying about their medication usage, in some way? Involvement in doctor shopping is another sign of dependency, as the individual attempts to obtain several prescriptions, past what a professional would find safe to prescribe.
What Can Be Done to Lessen the Effects of Suboxone?
As with any medication, there is a level of risk management involved in administration. If you choose to take the proper safety precautions, you can reduce your risk of experiencing complications while taking Suboxone.
Some important precautions that you should be taking are:
- Before you begin another new medication (other than Suboxone), make sure to confirm with your doctor that this is safe.
- Avoid ingesting or consuming anything that can lead to slowed breathing; this includes alcohol, sedatives, tranquilizers, or certain drugs.
- If you have any liver-related health problems, ensure that your doctor is aware of this before starting a Suboxone regime.
- Let your doctor know if you are currently pregnant or if you plan on becoming pregnant.
- Avoid using Suboxone as a long-term solution, and instead, limit its use to the detox phase of opioid addiction recovery.
As long as you abide by these precautions, you can lower your risk of becoming physically and psychologically dependent upon Suboxone; you will also lower the likelihood that you develop other severe side effects or complications.
Medication Assisted Treatment for Opioid Addiction

If you are currently seeking out treatment for opioid addiction, it’s vital that you’re cared for by professionals with experience. Opioid addiction is a complicated disorder, and as a consequence, the process of healing can also be highly complex. Plus, no one method of treatment is going to work for everyone; instead, it is important that each and every patient receive personalized treatment tailored to their unique needs and circumstances.
We offer medication-assisted treatment (MAT) services including Suboxone and Vivitrol. Our goal is to find the right treatment for your needs. If that means using Vivitrol and Suboxone to help a client wean off of other drugs, we certainly will recommend MAT.
Our professionals will assess your situation and develop a customized treatment plan with a personalized mix of holistic and clinical services for your recovery.
If you’re interested in learning more about Maryland Recovery, call anytime to talk to our experienced staff. We’re here 24/7 to answer any questions you have. (877) 762-3766
Reviewed by Christopher Schwartfigure MS, LGPC, CAC-AD








