 Substance abuse and mental illness often go hand-in-hand. According to the Substance Abuse and Mental Health Services Administration, people with mental illness are more likely to have a substance abuse or addictive disorder than people who are not mentally ill. This is called a co-occurring disorder, or dual diagnosis.
Substance abuse and mental illness often go hand-in-hand. According to the Substance Abuse and Mental Health Services Administration, people with mental illness are more likely to have a substance abuse or addictive disorder than people who are not mentally ill. This is called a co-occurring disorder, or dual diagnosis.
Co-occurring disorders can be difficult to diagnose because addiction or substance abuse may be masking its symptoms. Substance abuse and mental health disorders are complex medical conditions that vary in severity. It’s not uncommon for people to receive treatment for one disorder, while the other goes untreated. Patients with co-occurring disorders in which one goes undiagnosed or untreated are more likely to experience incarceration, homelessness, suicide, and premature death.
How Common Is Dual Diagnosis?
Dual diagnosis is more common than you might think. In 2014, there were an estimated 8 million people in the United States with a co-occurring mental health and substance abuse disorder. Patients with co-occurring disorders have the best chance with integrated treatment options. In dual diagnosis treatment, health care providers address mental health and substance abuse disorders at the same time, which creates better outcomes. Statistically, those with the best outcomes receive dual diagnosis therapy with early detection and treatment. Dual diagnosis therapy significantly improves quality of life for the patient and their families.
Dual Diagnosis and ADHD
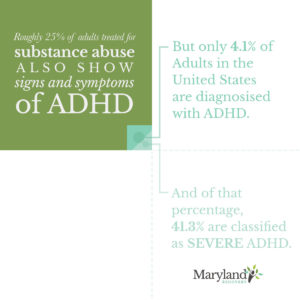
Substance abuse is particularly risky if you have attention-deficit/hyperactivity disorder (ADHD). A recent survey found that adults with ADHD experienced alcohol or drug dependence at a rate 3 times that of the general population. Statistically, men with ADHD are slightly more likely to abuse alcohol than women – 21 percent compared to 13 percent.
Those afflicted with ADHD are more vulnerable to substance abuse for several reasons. First, ADHD can create a negative impact on academic and work performance, as well as social interactions. To combat these effects, people with ADHD may turn to substance abuse. Secondly, addiction may be a consequence of biology. People with ADHD have naturally less dopamine than those without ADHD, and using drugs or alcohol triggers a temporary rush of this endorphin.
A Many-Pieced Puzzle
Another difficulty in treating ADHD is the fact that medications prescribed to treat it can become habit-forming. Commonly prescribed stimulants such as Ritalin and Adderall are effective at managing some of ADHD’s symptoms, but they are also easy to abuse.
ADHD varies from person to person, but in general, patients demonstrate an inability to focus, constant physical activity, and impulsive behavior. Patients may have difficulty completing tasks, listening to others, organizing, or following directions, and may be easily distracted. This leads to problems at work, as well as in interpersonal relationships. Drugs and alcohol may provide people with ADHD an outlet to relax and slow down so they can fit in socially.
The Importance of Dual Diagnosis Therapy
 ADHD and addiction are treated simultaneously in a dual diagnosis setting. It’s imperative to treat these two conditions at once, as the cycle of mental illness leads to alcohol or drug abuse, and vice versa. One condition is continually exacerbating the other. Holistic treatment for ADHD includes counseling, self-help therapy, family and group therapy, and holistic interventions that treat both the body and the mind. Patients must have access to a supportive environment that allows them to heal and enjoy life after the initial recovery process.
ADHD and addiction are treated simultaneously in a dual diagnosis setting. It’s imperative to treat these two conditions at once, as the cycle of mental illness leads to alcohol or drug abuse, and vice versa. One condition is continually exacerbating the other. Holistic treatment for ADHD includes counseling, self-help therapy, family and group therapy, and holistic interventions that treat both the body and the mind. Patients must have access to a supportive environment that allows them to heal and enjoy life after the initial recovery process.
A dual diagnosis program, in particular, emphasizes modifying the destructive thoughts and behaviors that create substance abuse. In people with ADHD, impulse control is one of the most important components of intervention. Since people with ADHD often have trouble navigating social situations, building self-esteem is also an important aspect of recovery.
Therapists will also work with individuals to help them identify their triggers and what leads them to abuse drugs or alcohol. They also educate families and support systems on the realities of living with ADHD, and how they can help throughout the recovery process.
Why Dual Diagnosis Therapy Works
Dual diagnosis therapy programs simultaneously manage the symptoms of an individual’s ADHD and help them discover modifications and triggers throughout the initial recovery. Over time, individuals will begin to recognize those triggers within themselves and modify their behavior accordingly. This will give a person living with ADHD and addiction the ability to live a happy, healthy life without having to depend on substances such as drugs or alcohol.
ADHD Still Goes Under-Diagnosed
If you know someone who struggles with a substance abuse disorder, there is a chance they may have ADHD, even if they have never been diagnosed. ADHD is an under-diagnosed and misunderstood disorder that has a complex etiology. While genetics plays the largest role in the onset of ADHD, researchers have also found a connection between mothers who use alcohol or smoke during pregnancy and ADHD in their offspring. Lead exposure may also be linked to ADHD. Although rare, ADHD can result from traumatic brain injury or stroke.
If you or someone you love is struggling with addiction and exhibits these symptoms, talk to a treatment provider. It’s not uncommon for treatment centers to uncover co-occurring mental disorders throughout the course of treatment.
ADHD and substance abuse are both complex conditions. As such, they must be treated efficiently and with a tailored approach. Dual diagnosis therapy offers the best chance for individuals suffering from these conditions to lead productive, fulfilling lives.
A Full Recovery From Substance Abuse Includes Ensuring Positive Mental Health and Stability
START YOUR FULL RECOVERY WITH MARYLAND RECOVERY:
Read More About the Warning Signs
Reviewed by Christopher Schwartfigure MS, LGPC, CAC-AD








