 Statistics in Maryland paint a dismal picture of emergency room visits for alcohol and drug addiction in the Old Line State and around the country. Substance abuse has long been a problem in the United States, but recent statistics reflect the remarkable, mind-blowing overdose rates.
Statistics in Maryland paint a dismal picture of emergency room visits for alcohol and drug addiction in the Old Line State and around the country. Substance abuse has long been a problem in the United States, but recent statistics reflect the remarkable, mind-blowing overdose rates.
The rate of opioid-related overdose deaths has more than quadrupled since 1999, and alcohol-related causes are the fourth leading preventable cause of death in the country. Approximately 88,000 people die every year from alcohol-related causes, while prescription and illicit drugs take the lives of at least 40,000 more. Every state is feeling the effects of this unusual problem, and Maryland is no exception. Emergency department statistics give a comprehensive overview of the issue here.
A Glimpse of the Drug and Alcohol Problem in Maryland
The Maryland Department of Health and Mental Hygiene released a report in September 2015 summarizing drug- and alcohol-related emergency visits in Maryland from 2008 to 2014. The report used data the Maryland Health Services Cost Review Commission (HSCRC) collected from discharge medical records for the more than 2 million people who visited the hospital annually. According to the report, in 2014 there were 11,242 drug- and alcohol-related emergency room (ER) visits in Maryland. Baltimore had the highest rate of ER visits, more than double the statewide average.
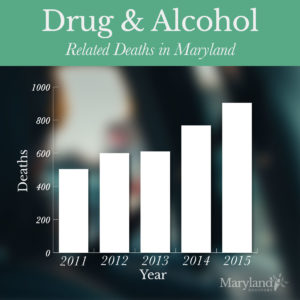
Data from the third quarter of 2016 shows staggering numbers of drug- and alcohol-related deaths – the highest in years. From January to September, 1,468 people died from drugs or alcohol in Maryland. The data compares to far fewer deaths in the same period in previous years:
- 2015 – 904 Deaths
- 2014 – 767 Deaths
- 2013 – 610 Deaths
- 2012 – 600 Deaths
- 2011 – 504 Deaths
There were 465 overdose deaths in 2010, a 10-year low. Almost every county in Maryland saw a rise in intoxication-related deaths from 2015 to 2016. The only exceptions were Garrett, Somerset, and Washington Counties, where rates dropped. The most deaths occurred in the City of Baltimore, with 291 in 2015 and 481 in 2016. These statistics represent a major ongoing problem in the state.
Prescription opioids killed 317 people in Maryland from January to September 2016, an increase from 270 overdose deaths in 2015. Growing prescription opioid abuse has led to a consequent rise in heroin abuse. Of the 317 opioid-related deaths in 2016, 163 were in combination with heroin and/or fentanyl. The steady rise in overdose deaths in Maryland showcases the ongoing drug and alcohol abuse problem plaguing the entire country.
The Source of the Problem: What Causes Addiction?
To get to the bottom of the substance abuse issue in Maryland, one must understand the nature of addictions. There are many misconceptions surrounding addiction that perpetuate stigmas and make it more difficult for addicts to receive the help they need. According to most medical associations, drug and alcohol abuse is not a matter of morals it’s a disease of the body and brain. Perceiving this issue as a disease can help recovery and rehabilitation efforts address the correct ways to stop addictions.
Drugs and the Brain
Drugs alter critical areas of the brain that are necessary for functions such as eating, breathing, driving, and everyday activities. Drugs affect the brain stem, the cerebral cortex, and the limbic system. The limbic system is the brain’s reward center, which controls the ability to feel pleasure. Drug abuse triggers the limbic system and eventually makes it difficult or impossible for the user to feel pleasure when not on drugs. Drugs’ effects on the limbic system are major constituents in the perpetuation of addiction.
Drugs are chemicals that tap into the brain’s communication system and interfere with the way neurons process information. These drugs lead to a five-step process that ultimately create a substance addiction:
- The brain’s receptors mistake drug chemical structures for neurotransmitters, allowing them to attach and activate the neurons.
- Drugs don’t activate the neurons the way natural neurotransmitters do, leading to abnormal messages within the brain.
- At the same time, most addictive drugs flood the brain’s reward system with dopamine – a neurotransmitter that naturally exists in the mind. Dopamine is responsible for regulating feelings of pleasure, as well as emotion, motivation, and movement.
- Overstimulation of the brain’s reward system with drugs and additional dopamine produces euphoric effects. The brain then associates the drug with pleasure and reward, teaching the user to do it again and again to achieve the same results.
- Over time, regular drug use will reduce the reward circuit of the brain’s ability to experience pleasure at all. The user cannot enjoy things that were once pleasurable, such as eating or sex. Now, the user can only achieve normal dopamine function with drug use.
By this point, the brain is conditioned to the drug and has a higher tolerance for the chemicals. A vicious cycle occurs, where the user has to consume much larger amounts of the drug to produce the familiar high. This is where abuse and overdose come into play.
Alcohol and the Brain
Alcohol also affects the brain, but in different ways than other drugs. Alcohol alters the levels of neurotransmitters in the brain, increasing inhibitory transmitters that decrease brain activity. Liquor is what causes slurred speech and slow movements. Alcohol also suppresses the neurotransmitter glutamate, which contributes to stimulating brain activity. The suppression results in the further physiological slowdown. At the same time, alcohol increases dopamine levels in the brain, creating the pleasurable feeling that comes with drinking. Drunkenness is a combination of unnatural changes within the brain.
Alcohol affects the brain’s cerebral cortex, cerebellum, and medulla as well as the hypothalamus region and pituitary gland. These areas of the brain control almost every aspect of the human body, including vital behaviors and processes including:
- Thought and Information Processing
- Movement and Balance
- Brain Functions and Hormone Release
- Sexual Arousal and Performance
- Breathing
- Body Temperature
- Consciousness
Excessive short-term alcohol use can cause blackouts and short-term memory loss, as it acts on the medulla and induces sleepiness. Alcohol abuse in the long term, however, can permanently damage areas of the brain – not to mention the damage it causes to the heart, liver, and pancreas. Perpetual alcohol consumption will eventually cause the brain to shrink and suffer a deficiency in the fibers that carry information inside the brain. Alcohol also decreases thiamine, a B vitamin, in the brain, leading to a condition called Wernicke-Korsakoff syndrome. People with this condition suffer mental confusion, lack of coordination, and memory and learning problems.
Roadblocks to Recovery
The more scientists learn about the effects of drugs and alcohol on the brain, the more they understand the difficulties and barriers to addiction recovery. Maryland’s rampant increase in emergency room visits related to drug overdose and alcohol-related health problems points to an issue in current treatment and rehabilitation efforts. Understanding the most prominent roadblocks for those on the road to recovery can shed light on why emergency room statistics continue to surge at record-breaking rates.
 The people who are suffering are people who have become dependent on a substance for daily life – often for total functionality. The brain has become dependent on the drugs and/or alcohol, and no longer knows how to function without it. When an addict stops or reduces his or her consumption of drugs and alcohol, it puts the brain through withdrawal.
The people who are suffering are people who have become dependent on a substance for daily life – often for total functionality. The brain has become dependent on the drugs and/or alcohol, and no longer knows how to function without it. When an addict stops or reduces his or her consumption of drugs and alcohol, it puts the brain through withdrawal.
Withdrawal is an incredibly difficult phase of addiction recovery, and can even cause death in an unsupervised setting. It’s essential for addicts to go through withdrawal in the right rehabilitation facility or hospital. Withdrawal is the brain struggling to readjust its chemistry. The process can cause hallucinations, disorientation, delirium tremens, sweating, nausea, and seizures.
Those affected need a lot of help during recovery but often cannot get the assistance they need in time to prevent a relapse or deadly overdose. Maryland’s lack of facilities to accommodate those going through withdrawal and detoxification is perpetuating addictions, leading many to feel hopeless. They often end up in Maryland’s emergency rooms, costing taxpayers millions in health care costs every year. Studying substance-related ER visits in the state could give policymakers a deeper insight into this massive epidemic.
Maryland Drug- and Alcohol-Related Emergency Visit Data
Drug- and alcohol-related emergency department visits have to code as any visit to a Maryland specialty hospital or emergency facility, leading to a drug or alcohol ICD-9 code, in the diagnosis position on the record. This code is the primary medical condition the location treated during the patient’s visit. Each record included in the study from 2008 to 2014 had an ICD-9 code in the diagnosis position and up to 28 of these codes in the secondary diagnosis area. The presence of an ICD-9 code in any spot represents a visit related to intoxication, substance poisoning, or toxic effect. The report classifies six different categories of emergency visits:
Drug- and Alcohol-Related Visits
This category encompasses all records that contain one or more ICD-9 diagnosis codes for alcohol, benzodiazepine, cocaine, heroin, or prescription opioids. The total number of drug- and alcohol-related emergency visits in Maryland from 2008 to 2014 was 69,366 visits. The age-adjusted rate for these visits increased by 37.5% during this six-year period. A year-by-year breakdown of this data across Maryland is:
- 2008 – 7,779 Visits
- 2009 – 8,111 Visits
- 2010 – 8,737 Visits
- 2011 – 10,227 Visits
- 2012 – 12,062 Visits
- 2013 – 11,208 Visits
- 2014 – 11,242 Visits
The HSCRC organized this data according to trends such as race, ethnicity, age, sex, county, and type of substance. All around, the rates of drug- and alcohol-related emergency visits were highest among non-Hispanic White people, men, and people between the ages of 45 and 64. Data records show that drug- and alcohol-related visits were most frequent among individuals with Medicaid compared to other types of health care coverage.
County-By-County Breakdown
The counties with the most visits in the western area of Maryland was Montgomery County, with 7,833 visits from 2008 to 2014. In the central area, the largest number was in the City of Baltimore with 16,073 visits. Southern Maryland’s busiest County was Prince George’s County, with 6,063 visits. The Eastern Shore area’s major County was Wicomico County (1,788 visits), with Cecil County a close second (1,752 visits). The counties with the lowest numbers of drug and alcohol-related emergency visits were:
- Western Area – Garrett County 295 Visits
- Central Area – Howard County 1,700 Visits
- Southern Area – Charles County 1,251 Visits
- Eastern Shore Area – Kent County 252 Visits
According to county data for the total number of drug- and alcohol-related visits in Maryland, the City of Baltimore consistently had the highest rates of all the counties in the state. The study treats Baltimore as equal to a county for most purposes, despite it being an independent city rather than a county.
Baltimore had the highest number of ER visits for drug and alcohol issues and had a significant number of residents below the federal poverty line. In 2014, 144,849 people in the City of Baltimore were living below the poverty line of $23,850 for a family of four. The same year, 49.7% of city’s residents lived with incomes below 50% of the poverty line, at just $5,835 per year for an individual. Baltimore’s large population and percentage of people living in poverty contributed to this city’s staggering number of drug- and alcohol-related ER visits.
The Comorbidity of Drugs and Alcohol
It’s important to realize the influence of alcohol on drug-related visits. Drug and alcohol abuse are comorbid conditions, often working together in the same person. In 2014, more than half (53%) of all alcohol-related intoxication deaths in Maryland also dealt with heroin. The majority of drug- and alcohol-related emergency department visits in Maryland involve alcohol poisoning. Alcohol is a major factor that influences these types of ER visits.
From 2012 to 2013, the decrease in the total number of drug- and alcohol-related visits, reflective of an alcohol-related visit decline for the same years. From 2014, the number of drug- and alcohol-related visits stayed relatively the same, but take out alcohol-related visits and the number of drug-related visits drops. There were 6,282 visits related to drugs only, and 11,242 visits involving drugs and alcohol in 2014. Understanding the role of alcohol in Maryland’s drug problem will help rehabilitation facilities learn the nature of these addictions.
Alcohol-Related Visits
Alcohol-related visits in the study were those marked by one or more ICD-9 codes for alcohol intoxication, poisoning, or toxic effects. From 2008 to 2014, there were 34,416 alcohol-related emergency department visits in Maryland. During this time, the age-adjusted rate increased by 21%. Here’s a year-by-year breakdown of visits related to alcohol:
- 2008 – 4,015 Visits
- 2009 – 3,925 Visits
- 2010 – 4,559 Visits
- 2011 – 5,049 Visits
- 2012 – 6,190 Visits
- 2013 – 5,575 Visits
- 2014 – 5,103 Visits
Alcohol-related visits have increased since 2008, but not as swiftly as the number of alcohol- and drug-related visits combined. For the most part, rates have remained somewhat steady, peaking in 2012 and slowly dropping since then. Trends in alcohol-related emergency department visits exist and are similar to trends in alcohol and drug-related visits. Nearly half of all alcohol-related visits were individuals between the ages of 45 and 64. The number of men visiting the ER for alcohol-related reasons was more than triple the number of women in this period:
- 2008 – 3,012 Men |1,003 Women
- 2009 – 2,953 Men | 972 Women
- 2010 – 3,512 Men | 1,047 Women
- 2011 – 3,875 Men | 1,174 Women
- 2012 – 4,703 Men | 1,487 Women
- 2013 – 4,272 Men | 1,303 Women
- 2014 – 3,727 Men | 1,376 Women
Non-Hispanic Whites consistently made up the majority of alcohol-related emergency visits every year, followed by non-Hispanic Blacks and then Hispanics. In 2014, there were 2,701 non-Hispanic Whites, 1,356 non-Hispanic Blacks, and 453 Hispanics who visited the hospital due to alcohol-related reasons. The county with the highest number of this type of visit was again the City of Baltimore, with 8,765 total visits from 2008 to 2014. The county with the lowest number was Kent, with 60 visits. Kent County saw fewer than ten visits in 2008, 2010, 2011, and 2014.
Alcohol-related emergency department visits cost Maryland about $7.2 million in 2014, the same amount as in 2013. Expenses hit a six-year high in 2012 at $7.7 million and a record low for the same six years in 2008 at $3.3 million. In 2014, the expected payer for these visits in Maryland was mainly Medicaid, followed by commercial insurance, self-pay/no charge, and Medicare. Alcohol is a major contributor to all drug- and alcohol-related emergency visits and needs particular attention alongside anti-drug campaigns in Maryland.
Benzodiazepine-Related Visits
The drug categories of this study are broken down into benzodiazepines, cocaine, heroin, and prescription opioids. Benzodiazepines include Xanax, Valium, Lorazepam, and Restoril. Benzodiazepines affect the central nervous system, acting on the brain’s gamma-aminobutyric acid-A (GABA-A) receptors. These drugs enhance the brain’s response to GABA, opening GABA-activated channels and letting chloride ions enter. The drug causes the neuron to resist excitation. Doctors may prescribe benzodiazepines as sedatives, anticonvulsants, and muscle relaxants.
From 2008 to 2014, Maryland emergency departments received around 4,000 visits related to benzodiazepines – 2012 had the highest rates, with 735 people, while 2008 had the lowest with 376 people. In 2014, rates dropped slightly from the previous two years, with 601 benzodiazepine-related visits. In every year, non-Hispanic White people far outnumbered non-Hispanic Black people regarding benzodiazepine-related ER visits.
Benzodiazepines are one drug where female visits often equaled and outnumbered male visits. In 2008, 166 men visited compared to 210 women. Women outnumbered men again in 2010 (239 men, 291 women), 2011 (297 men, 352 women), and 2014 (298 men, 303 women). Doctors tend to prescribe benzodiazepines more often to women than to men for anxiety-related conditions. Many people are unaware of the addictive nature of benzodiazepines and start misusing these drugs even with legitimate prescriptions.
Age groups also departed from the trends for total drug- and alcohol-related visits, with 25- to 44-year-olds making up the highest number every year instead of 45- to 64-year-old people. In 2014, 261 visits were ages 25 to 44, compared to 186 45- to 64-year-olds. Benzodiazepine-related emergency visits cost Maryland about $0.88 million in 2014, paid for mostly by Medicaid. The primary residence for the people in these visits was Baltimore (776 visits total), while the average age-adjusted rate per 100,000 people put Cecil County in the lead at 28.1.
Cocaine-Related Visits
While cocaine has valid medical purposes, including as a local anesthetic for surgeries, it’s an illegal drug. Cocaine is a powerful stimulant that’s highly addictive. Like most addictive drugs, cocaine works by flooding the brain’s receptors with dopamine, the chemical in charge of feeling pleasure and movement. Cocaine prevents the natural recycling of dopamine in the brain, shutting off the signal between nerve cells instead of sending the dopamine back to the cell that released it. It causes excessive amounts of dopamine to build up in the brain, disrupting normal communication and causing the great sensation.
Cocaine can lead to bizarre and unpredictable behavior, especially in large amounts. It can make a person feel extreme, euphoric happiness and mental alertness, as well as hypersensitivity to light and sound. Many people also experience irritability, paranoia, and violent behaviors. The effects of cocaine appear immediately and can disappear within a few minutes to an hour depending on the method of use. Users may snort, inject, or smoke cocaine. The long-term effects of this drug can include malnourishment, bowel decay (when consumed by mouth), and movement disorders such as Parkinson’s disease.
 Cocaine overdoses can occur on a person’s very first use of the drug or at any use after that. When combined with alcohol or heroin, the risk of cocaine overdose significantly increases. Overdose can impact the blood vessels and heart, leading to a heart attack. It can also affect the body’s nerves, causing seizures and strokes.
Cocaine overdoses can occur on a person’s very first use of the drug or at any use after that. When combined with alcohol or heroin, the risk of cocaine overdose significantly increases. Overdose can impact the blood vessels and heart, leading to a heart attack. It can also affect the body’s nerves, causing seizures and strokes.
In Maryland, there were 1,106 cocaine-related emergency department visits from 2011 to 2014. Once again, 2012 had the highest amount in the study with 335 visits. This number dropped to 245 in 2013 and rose slightly in 2014 to 251 visits. The demographics for cocaine-related ER visits were mostly male, non-Hispanic Black people at ages 45 to 64. More than twice as many men as women were seen for cocaine-related reasons every year from 2011 to 2014. The same applies to the number of non-Hispanic Whites versus non-Hispanic Blacks.
The charges for cocaine-related emergency department visits from 2011 to 2014 were near $3.5 million. In 2014, Maryland spent $0.82 million on these kinds of visits. The primary expected payer of cocaine-related emergencies in 2014 was Medicaid. The City of Baltimore saw the highest number of these visits in the age-adjusted rate, at 16.7. The second-place County, Wicomico, was far behind Baltimore with just 6.5 per 100,000 people.
Heroin-Related Visits
Prescription opioids and heroin often go hand in hand. Consequently, the country has seen a marked increase in heroin abuse alongside the increase in opioid problems. In Maryland, heroin-related emergency visits reached a six-year high of 1,564 in 2014. The lowest year, 2008, saw only 301 heroin-related visits. This significant jump in just six years showcases the out-of-control presence of heroin in Maryland and around the United States. Here’s a year-by-year breakdown:
- 2008 – 301 Visits
- 2009 – 514 visits
- 2010 – 346 visits
- 2011 – 429 visits
- 2012 – 815 visits
- 2013 – 1,124 visits
- 2014 – 1,564 visits
In 2014, Maryland had 26.4 heroin-related department visits per 100,000 people. Regarding gender, males outnumbered females consistently in every year of the study. This discrepancy was significant in 2014, with 440 female visitors compared to a large 1,124 male subjects. Non-Hispanic White people were much more widespread than non-Hispanic Black people. The latter made up 254 heroin-related visits in 2014, while the former made up 873 visits. The most prominent age group in this category was 25- to 44-year-olds, followed by 15- to 24-year olds.
Maryland paid about $1.55 million for heroin-related emergency visits in 2014, a jump from $1 million in 2013. The expected payer for these visits was self-pay/no charge up until 2014 when the expected payer jumped to Medicaid. In 2013, self-pay/no charge made up 433 visits, while Medicaid paid for 389 visits. In 2014, this data was drastically different – self-pay/no fee paid for about 363 visits while Medicaid paid for about 792 visits. Baltimore (the city) had the highest rate of heroin-related ER visits in both number and age-adjusted rate per 100,000 people.
Prescription Opioid-Related Visits
Prescription opioid abuse is an epidemic in the country, and Maryland has not escaped unscathed. Prescription opioids are a viable way to treat Americans suffering from chronic pain. Unfortunately, painkillers are also addictive. A legitimate medical issue can quickly turn into a substance abuse problem with prescription opioids such as morphine, methadone, hydrocodone, oxycodone, and buprenorphine. Brand names for these drugs include OxyContin, Percocet, Vicodin, and Demerol.
From 1999 to 2015, more than 183,000 people died in America from prescription opioid overdoses – 2015 alone saw more than 15,000 such deaths. The death toll has more than quadrupled since 1999, relative to sales increases for these drugs. Each day, national emergency departments treat more than 1,000 people for misusing prescription opioids. This issue has become rampant around the country, leading to a national call for changes in opioid prescribing practices.
The greater availability and lack of awareness regarding prescription opioid addiction has led to a marked increase in related emergency room visits in Maryland. The rate of prescription opioid-related emergency department visits has increased since 2008, hitting a six-year high in 2014 with 1,101 total visits. Look at the numbers year by year to track the growing trend:
- 2008 – 512 Visits
- 2009 – 710 Visits
- 2010 – 787 Visits
- 2011 – 921 Visits
- 2012 – 1,083 Visits
- 2013 – 1,006 Visits
- 2014 – 1,101 Visits
Within this data, men made up more of the visits than women did, but not by a wide margin. In 2014, 616 men visited the ER for prescription opioid-related reasons, compared to 484 women. The margin was the lowest in 2011, with just 29 more male visitors than female ones. Regarding ethnicity/race, non-Hispanic White people made up the majority of visitors every year. In 2014, 543 visits were by non-Hispanic White people compared to 246 non-Hispanic Black people.
The age group most likely to visit the ER for prescription opioid-related issues is 25- to 44-year-olds, followed by 45- to 64-year-olds and 15- to 24-year-olds. The cost of these emergency room visits in Maryland was $1.5 million in 2014, paid mostly by Medicaid. The City of Baltimore saw the highest number of prescription opioid-related emergency department visits concerning the actual number and age-adjusted rate. However, Cecil County was very close in age-adjusted rate, with 33.7 per 100,000 people compared to Baltimore’s 34.0.
Noticeable Data Trends
There are several trends apparent in the data for the total number of drug- and alcohol-related ER visits. There is a marked difference in the number of men versus the number of women in most addiction situations. In 2014, 7,183 people visited emergency rooms for drug- and alcohol-related reasons, compared to 4,058 women. Other than benzodiazepines, men accounted for a higher number of visits than women in every category.
Hope for the Future
Maryland recently initiated the Prescription Drug Monitoring Program (PDMP) to help put an end to prescription opioid abuse. Launched by the Department of Health and Mental Hygiene, the PDMP will collect and store information relating to patient painkiller prescriptions. The PDMP will enable investigators to find and stop illegal prescription and drug use activities in Maryland.
The PDMP is a step in the right direction for regaining control of the substance abuse problem in Maryland. Prescription opioids are just one category leading to emergency department visits in the state, and it links closely with other drug use – especially heroin. Ending prescription opioid abuse can cover significant ground toward an addiction-free future. It is everyone’s responsibility to spread awareness about substance abuse to help put a stop to this devastating issue for good.
Maryland Drug and Alcohol Addiction has Grown to Dangerous Levels, Don’t Let Drugs and Alcohol Ruin Your Life!
CALL OUR SPECIALISTS TODAY TO START YOUR RECOVERY:
Reviewed by Christopher Schwartfigure MS, LGPC, CAC-AD








